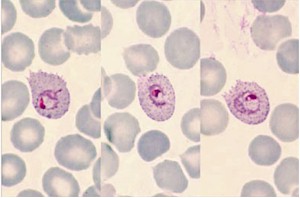
Fig. 258. Plasmodium ovale. Three typical trophozoites that make species diagnosis very easy
Image courtesy of the authors of Atlas of Human Malaria.
From Zeno Bisoffi and Giovanni Swierczynski, of the Centre for Tropical Diseases, S. Cuore Hospital, in Negrar (Verona), Italy.
At the recent ECTMIH 2009 in Verona, Italy, a very well attended parallel session discussed the problem of malaria diagnosis. The keynote lecture by Walter Wernsdorfer had the provocative title: The Use of Rapid Diagnostic Tools – the End of Traditional Microscopic Diagnosis of Malaria?
Not surprisingly, the speaker expressed serious concern about totally abandoning microscopy in favor of the "new" rapid diagnostic tests (RDTs), and fears that microscopy would become obsolete, although no real demonstration exists of the superiority of the new tools.
A hot debate followed.
Members of the audience argued that microscopy quality in Africa (and not only there!) is usually very poor, and that in any case RDTs are the only option where there is no laboratory. They suggested that RDTs should become "standard" in malaria diagnosis, in adults and children.
The subject remains controversial, however. We highlight the main issues that need to be addressed for RDTs below:
1. Recent research has shown that clinicians are reluctant to refrain from treating for malaria after a negative test (1-3). So far, there is no convincing evidence that adequate compliance with the (negative) test result can be uniformly achieved. Of course this is true for microscopy, too.
2. As Wernsdorfer said, RDTs do not allow a quantitative assessment of the parasite density: therefore, in settings where most people are carriers of malaria parasites, the test result will be almost invariably positive, and of no utility in differentiating a simple malaria infection from clinical malaria. Microscopy is not only quantitative, but also detects different stages (such as schizonts and young gametocytes) that are potential markers of severe disease.
3. The safety of an RDT-based approach, especially for young children, has not yet been convincingly demonstrated, though some encouraging indications have recently become available (4).
4. In areas with great seasonal differences in transmission intensity, a very sensitive test could be better when transmission/prevalence is low, and a less sensitive one when transmission is high and most are carriers of malaria parasites, but this is clearly not feasible in practice.
For these and other "grey areas", the utility (and safety) of a RDT-based approach to malaria management is still under debate, especially for children (5, 6).
As far as microscopy is concerned, it is unfortunately true that its quality in endemic countries (and not only there!) is far from satisfactory, to say the least! There are many reasons for this: lack of training, low quality of staining and sometimes of the microscopes, and no quality control. Is this a sufficient reason to abandon microscopy in favour of RDTs? We are not aware of any study comparing the cost-effectiveness of both methods (including a well organised quality control, which is, not only necessary for microscopy, but also for RDTs!).
Our personal opinion is that "old" microscopy should not be abandoned, and that huge efforts are needed to assure an adequate quality standard. In order to contribute to this purpose, we would like to introduce a comprehensive manual of malaria microscopy (7) (www.atlas-malaria.com), that can be used for teaching purpose and as a reference tool in laboratories.
REFERENCES
1. Reyburn H, Mbakilwa H, Mwangi R, Mwerinde O, Olomi R, Drakeley C, et al. 2007. Rapid diagnostic tests compared with malaria microscopy for guiding outpatient treatment of febrile illness in Tanzania: randomised trial. BMJ 334 (7590):403.
2. Lubell, Y., Reyburn, H., Mbakilwa, H., Mwangi, R., Chonya, S., Whitty, C.J., & Mills, A. 2008. The impact of response to the results of diagnostic tests for malaria: cost-benefit analysis. BMJ. 336, (7637), 202-205.
3. Bisoffi, Z., Sirima, B.S., Angheben, A., Lodesani, C., Gobbi, F., Tinto, H., & Van den, E.J. 2009. Rapid malaria diagnostic tests vs. clinical management of malaria in rural Burkina Faso: safety and effect on clinical decisions. A randomized trial. Trop.Med Int Health. 14, (5), 491-498.
4. Msellem, M.I., Martensson, A., Rotllant, G., Bhattarai, A., Stromberg, J., Kahigwa, E., Garcia, M., Petzold, M., Olumese, P., Ali, A., & Bjorkman, A. 2009. Influence of rapid malaria diagnostic tests on treatment and health outcome in fever patients, Zanzibar: a crossover validation study. PLoS Med. 6, (4), e1000070.
5. D'Acremont, V., Lengeler, C., Mshinda, H., Mtasiwa, D., Tanner, M., & Genton, B. 2009. Time to move from presumptive malaria treatment to laboratory-confirmed diagnosis and treatment in African children with fever. PLoS.Med. 6, (1), e252.
6. English, M., Reyburn, H., Goodman, C., & Snow, R.W. 2009. Abandoning presumptive antimalarial treatment for febrile children aged less than five years–a case of running before we can walk?PLoS Med. 6, (1), e1000015.
7. Swierczynski G., Gobbo M. Atlas of human malaria. ISBN 9788890289200 2007 Published by Az Color, Sirmione, Italy. Email: s.michelucci@azcolor.it
